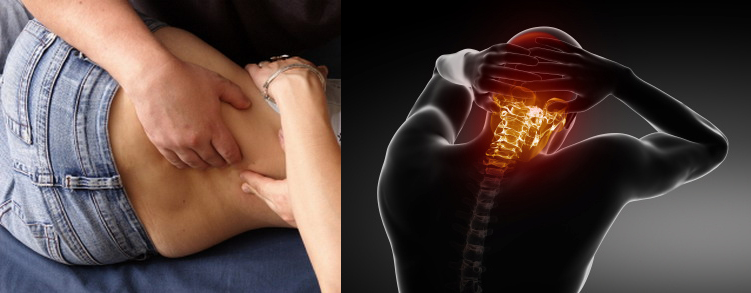
Lower back pain (LBP) can arise from many causes. Nearly everyone has or will suffer from LBP at some point in time, though it is most common in the 30-year-old to 50-year-old group and it affects men and women equally. However, what about the elderly population and low back pain? Let’s discuss back pain unique to the geriatric population…
We’ve all heard of the “wear and tear” factor as it applies to clothing, automobiles, shoes, and tires, but it affects our bones and joints too! A condition that none of us can fully avoid is called osteoarthritis (OA). OA is the “wear and tear” factor on our joints, particularly the smooth covering called hyaline cartilage located on the surfaces of all moving joints. It’s the shiny, silky smooth surface that we’ve all seen at the end of a chicken leg when we separate it from the thigh. Osteoarthritis is the wearing away of that shiny, smooth surface and it can eventually progress to “bone-on-bone” contact where little to no movement is left in the affected joint. Bone spurs can also occur and be another potential generator of back pain. OA is NOT diagnosed by a blood or lab test but rather by an accurate history, physical examination, and ultimately, an x-ray. However, when the low back is affected by OA, it may not even hurt! Yes, in some cases, there may be a significant amount of OA on an x-ray and that patient may not have significant problems. Or the opposite can occur and some patients with very little arthritis can have a lot of back trouble. It’s FREQUENTLY very confusing. The “take-home” message with OA is that, in and of itself, it does not always generate pain. This is why the history, physical examination, and the response to treatment (chiropractic adjustments, exercise, and possibly some lifestyle changes in diet and activity) are MORE important than the amount of arthritis found on the x-rays. Ultimately, we will ALL get OA sooner or later. It’s usually a slow, gradual process that may slowly change our activity level. Ironically, KEEP MOVING is the best advice we can give to the patient with OA.
There are a number of conditions associated with OA that affect the spine and respond well to chiropractic treatment. Degenerative disk disease (DDD) is one of those conditions found in association with OA. In fact, another name for OA is “degenerative joint disease” (DJD)! The normal anatomy of the intervertebral disk (IVD) consists of a thick, tough outer layer of fibroelastic cartilage and a central “nucleus” that is more liquid-like and allows the IVD to function like a shock absorber. As we age, the water content gradually “dries up” and the shock absorbing quality is lost.
As chiropractors, we address OA (DJD) and DDD with a number of HIGHLY EFFECTIVE treatments but most important (in many cases) is the use of spinal manipulation or adjustments. “Exercising the joint” with manipulation and mobilization reduces the tightness and stiffness associated with OA and DDD. Exercises are also important and can give the OA/DDD patient a way of controlling this condition on their own. Diet, activity modification/encouragement, and periodic adjustments help a lot! Next month, we will continue this discussion!
We realize you have a choice in whom you consider for your health care provision and we sincerely appreciate your trust in choosing our service for those needs. If you, a friend, or family member requires care for back pain, we would be honored to render our services.